If you live in the San Francisco Bay Area like me, you have been under shelter in place orders for the last week. With a minimum of two more weeks to go, our local economy and traffic have come to halt, and we are all adjusting to social distancing. Today, I will explain why we are sacrificing.
If you had never seen a model of a virus before the COVID-19 outbreak, now you know what they look like. Above is the depiction of the coronavirus from the CDC website.
Coronavirus Origin Story
So why do we care where the virus came from? Doctors are not lawyers or politicians, so we are not looking to lay blame. When we say origin, we don’t mean this is a Chinese virus, in fact, except for proximity, geography is not a priority. We do not care about the country of origin, but we do care about where it developed. Let me explain.
Viruses can develop in humans, or they can develop in other animals and then cross over to humans. This is critically important, because if the origin is humans, recurrent pandemics are unlikely. On the other hand, if the origin is in another animal species, there is an increased risk of future, large scale, re-emergence.
Currently, it is not clear if COVID-19 developed in humans or in another species. There are similarities and key differences and only additional investigation will sway scientific opinion. The only thing scientists have been consistent about is that this looks like a wild virus and a man-made, engineered virus.
COVID-19 is also known as SARS-CoV-2. If there is a 2, you would rightly assume that there was a 1. The 1 was SARS-CoV. Both have spike glycoproteins that bind to the ACE2 receptor on human cells. The spike is like the key and the receptor is like the door that the virus uses to enter. Similarities between the two viruses are evidence that SARS-CoV-2 mutated from SARS-CoV in humans. On the other hand, mutations in the spike proteins found on SARS-CoV-2 are also found in the virus that infects bats and pangolins, which would lend evidence supporting an origin in bats or pangolins. However, there are key differences in SARS-CoV-2 that to date have only been seen in human variations. More information is available in scientific language in Nature Medicine.
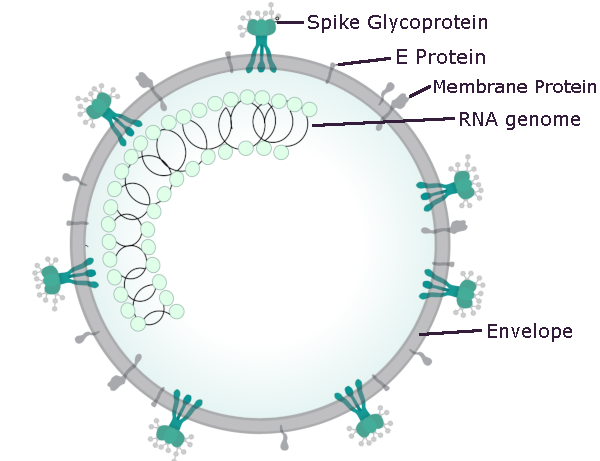
The structure of the coronavirus is illustrated in more detail above. The spike glycoprotein is the key that allows COVID-19 to enter via the ACE2 receptor in humans, ferrets and cats.
Wherever It Came From, It’s Here. Now What?
As every media outlet will tell you, the virus is here and spreading. Predictions are that 40-70% will become infected. Most people who contract the virus will have mild symptoms and recover fully, but 20% will have more serious symptoms and may require hospitalization. The goal is to slow the inevitable and have fewer people sick at once. The reason is that if everyone is sick at the same time, there will not be enough rooms, beds or ventilators in our hospitals to treat those in need, and more people will die.
COVID-19 Vaccine
The ideal treatment would be a vaccine to prevent infection in those who have never been exposed. Although several clinical trials are underway to develop a vaccine for COVID-19, the peak of this crisis will likely be over before a proven vaccine is available.
COVID-19 Medicines
Currently, there are no medications available to stop the virus. Rumor abound regarding meds that may help mediate the bodies response to the virus, but these still require studies to determine if they are safe and effective.
Medications under investigation that may help reduce COVID-19 infections include colchicine – an anti-inflammatory, chloroquine – an antimalarial and azithromycin – an antibiotic, but I cannot emphasize enough that the safety and efficacy of these proposed treatments have not been established.
Drugs that may worsen COVID-19 infections may include ibuprofen (the WHO has flip-flopped on this one), ACE inhibitors and angiotensin receptor blockers. The thought is that these meds may increase the ACE2 receptors in the lungs and provide more portals of entry for the COVID-19 virus. These also are hypotheses, with only anecdotal evidence and at this time, have not been proven.
COVID-19 Basic Prevention
We are left with the basics when dealing with a novel infectious agent. Since the primary method of transmission is via droplets from sneezing/coughing, physical methods to block droplet transmission is paramount. The best method is stay away from anyone with the virus, thus the shelter in place orders. If you are going to come into contact with other humans, the next best barrier is for everyone with the disease to wear a mask. Third best is for everyone without the disease to wear a well fitted respirator. Loose fitting masks seem to provide little protection.
Wash Up
If you prevent the direct inhalation of droplets from the air, the next line of defense is to prevent the transmission via surfaces. The virus is able to live for some time on many different surfaces. If you touch these surfaces, and then touch your face, you are likely to inoculate yourself. This is why so much emphasis has been placed on hand washing and cleaning. It’s not new, improved or sexy, but just like the standard, tried and true facelift, we do it because it works. The amount of time virus can remain viable is variable. Current estimates are in aerosols for up to three hours, four hours on copper, 24 hours on cardboard and 2-3 days on plastic and stainless steel.
Isolation After Exposure
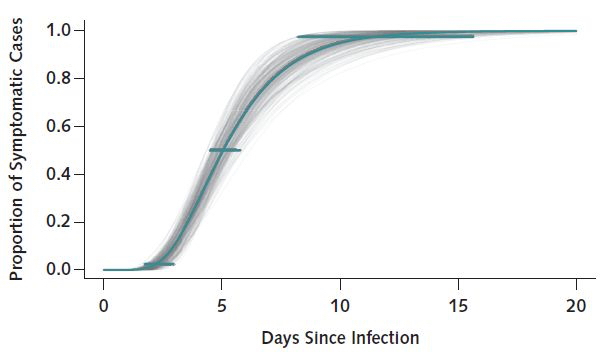
Above is a graph showing the number of days it takes to develop symptoms after exposure to the COVID-19 coronavirus.
The graph above depicts the number of days it takes to develop symptoms after exposure to the COVID-19 coronavirus. On average, half the exposed patients will develop symptoms in the first five days. 99% of patients will show symptoms by 14 days. This is why the quarantine is 14 days. If this seems long, remember the origin of the word quarantine – a period, originally 40 days, of detention or isolation imposed upon ships, persons, animals, or plants on arrival at a port or place, when suspected of carrying some infectious or contagious disease.
What Are The Symptoms of COVID-19?
Common symptoms of coronavirus infections include fever, cough, and shortness of breath. Muscle pain, sputum production, diarrhea, sneezing, runny nose, sore throat, loss of taste and smell are less common.
The standard method of diagnosis is by reverse transcription polymerase chain reaction (rRT-PCR) from a nasopharyngeal swab. The infection can also be diagnosed from a combination of symptoms, risk factors and a chest CT scan showing features of pneumonia.
Current Goals For COVID-19
This animation from Wikipedia shows the effect of stopping the spread.
Stopping the Spread seems unlikely at this point in time, and it is only a temporary solution. Stopping the spread reduces the number of people initially exposed, but eventually another spike in cases occurs when the containment is breached. If it can be stopped long enough for a cure or a vaccine to appear great, If not, eventually everyone gets exposed.
This animation from Wikipedia shows the effect of flattening the curve.
Flattening the Curve is not stopping the spread as much as it is slowing the spread. The same number of people will become infected, but the goal is that not everyone gets sick at once. When successful, the number of cases present at any one time will not exceed our ability to care for the ill. In the case of COVID-19, the limit for treating the severely ill may be the number of ICU beds and ventilators available.
For perspective, if half the population of the US gets sick and 5% require a ventilator, we would need 7.5 million ventilators. This is a conservative guess, but assumes the entire population gets sick at once. We only have 150,000 ventilators in the US currently. If we can blunt the curve so that fewer than 150,000 people need a ventilator at once, we will have the resources to keep up, and there will be fewer deaths from coronavirus. On the other hand, if we don’t blunt the curve, a lot more people will die, and doctors are going to have to make very difficult decisions. For a look at the current world totals visit the John Hopkins Coronavirus Resource Center.
Future Planning
For now, flattening the curve is still in our hands. We can do it by sheltering in place; practicing social distancing, and weathering this storm. It would easier if our leaders could quit their partisan bickering and instead support us in our efforts. Perhaps, the independent media can begin to direct their reporting away from rumor, speculation and blame and toward how we can expand our healthcare system to better handle these inevitable surges in utilization. History is punctuated with pandemics worse than this one, and they will certainly occur again in the future.
Previous Post Next Post