Downsizing Breast Implants – What You Need to Know
Breast Augmentation remains the most popular elective cosmetic plastic surgery procedure and has one of the highest patient satisfaction ratings. The ability to provide […]
Breast Augmentation Options Breast Implants and Fat Grafting
Breast Implants have been around for 60 years, and Fat Grafting to the Breasts even longer. While Breast Augmentation with Breast Implants quickly, and […]
Breast Implant Maintenance and Breast Revision Surgery
Breast Augmentation Revision is used to maintain the aesthetic results of breast enhancing surgery. As we discussed last week, Breast Implants are not lifetime […]
Breast Implant Maintenance and Breast Revision Surgery
Breast Implants have come a long way over their 60 years of existence. They are available in a wider range of shapes, volumes and […]
Why Choose Breast Augmentation Near Me?
Breast Augmentation continues to be one of the most frequently requested cosmetic plastic surgery procedures. While Breast Implants have changed, the goals of Breast […]
Breast Implant Replacement Surgery
A week doesn’t go by without someone asking, “When do I need to replace my breast implants?” The simplest answer is, “When there’s a […]
Happy Patient = Happy Plastic Surgeon
It is an honor and a blessing to be a plastic surgeon. I get to practice medicine, one of the most challenging and stimulating […]
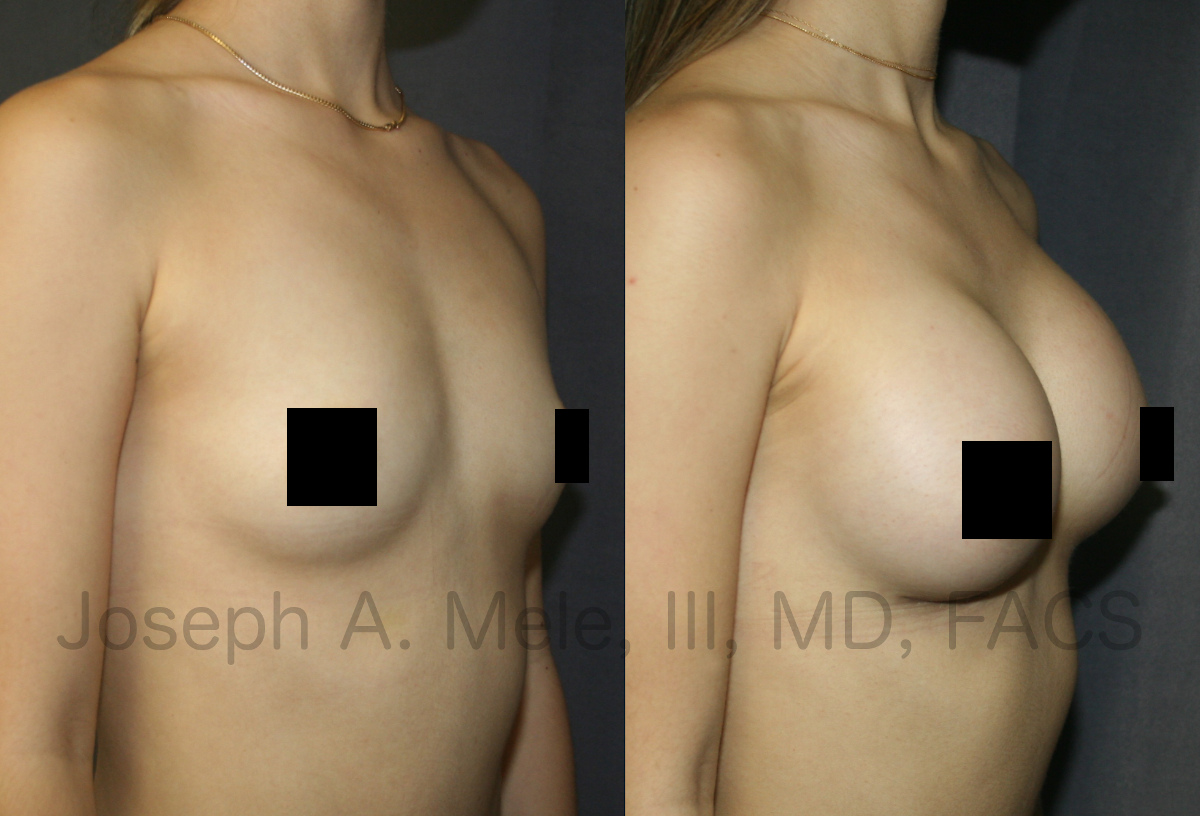
Spring Breast Augmentation. Which Breast Implants?
Spring is definitely in the air. The first day of Spring is this Friday, March 19th, and as winter winds down, the demand for […]
Breast Implant Revision Surgery Breast Augmentation Revision Video
Breast Augmentation Revision Surgery restores and corrects the appearance of Breast Implants that are not satisfactory. When Breast Implants deflate, move or become hard, […]
Breast Augmentation Revision Surgery Facts
Breast Augmentation remains one of the most requested Cosmetic Plastic Surgery procedures. It is important to remember that Breast Implants are not lifetime devices, […]